Freetown, Sierra Leone – December 2, 2025 – Sierra Leone’s Ministry of Health and Sanitation has disclosed that more than 81,000 individuals are currently living with HIV and AIDS, underscoring the ongoing challenge of the epidemic in the country despite significant strides in treatment and prevention.
The figure, shared by Health Minister Dr. Austin Demby, highlights the persistent burden of the virus in a country of approximately 8.8 million people, where the adult prevalence rate (ages 15-49) stands at around 1.7 percent, meaning roughly two in every 100 adults are affected. This equates to an estimated 78,000 to 81,000 people nationwide, with the majority (about 66,000) being adults over 15 and around 10,000 children under 14. Dr.
Demby, a veteran public health expert with decades of experience at the U.S. Centers for Disease Control and Prevention (CDC), emphasized during recent World AIDS Day commemorations that while the numbers remain concerning, Sierra Leone is on a path toward the global UNAIDS 95-95-95 targets by 2030, aiming for 95% of those living with HIV to know their status, 95% of diagnosed individuals on treatment, and 95% of treated people achieving viral suppression.
The announcement comes on the heels of encouraging progress reported just days ago on World AIDS Day (December 1).
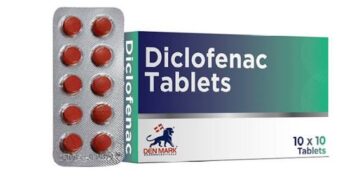
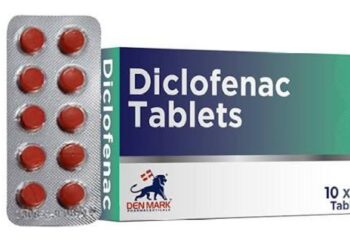
According to Sulaiman Lakoh, director of disease prevention and control at the ministry, AIDS-related deaths have plummeted by 73 percent, from 4,000 annually in 2022 to just 1,084 in 2025. This dramatic reduction is attributed to expanded access to antiretroviral therapy (ART), with 83% of people living with HIV now aware of their status and 83% of those diagnosed receiving treatment, as per the latest national data aligned with the Sierra Leone National Strategic Plan on HIV/AIDS (2021-2025).
Additionally, mother-to-child transmission has dropped by 43% over the same period, thanks to enhanced prenatal screening and ART linkage for pregnant women, 97.3% of HIV-positive mothers were connected to care in 2024 alone, per CDC-supported programs.
Sierra Leone’s HIV epidemic, first detected in 1987 among high-risk groups like sex workers, has been shaped by historical upheavals including a decade-long civil war (1991-2002) and the 2014-2016 Ebola outbreak, which disrupted healthcare and fueled transmission. The virus spreads primarily through heterosexual contact, with key populations, such as female sex workers, men who have sex with men, people who inject drugs, transgender individuals, and prison inmates, facing disproportionately higher rates, sometimes exceeding 10% in urban hotspots like Freetown.
Recent geospatial analyses from the 2019 Demographic and Health Survey reveal regional disparities, with higher prevalence in the Western Area (including the capital) compared to rural districts, driven by factors like poverty, migration, and limited testing.
Despite these gains, challenges persist. Nearly 40% of those infected remain undiagnosed, and stigma continues to deter testing and care, particularly among adolescents and young women, who account for a growing share of new infections, about 3,100 weekly in sub-Saharan Africa, with Sierra Leone contributing amid its low but rising national rate (up from 1.4% in 2022). Viral suppression rates hover at just 26% among adults, and even lower among youth, exacerbated by late-stage presentations where 70% of young patients arrive at clinics with advanced disease.
The ministry, in partnership with UNAIDS, the CDC’s PEPFAR initiative, and the National HIV/AIDS Secretariat, is ramping up efforts including community-led monitoring tools, adolescent-friendly services, and judicial dialogues to combat discrimination, as highlighted in a November 2023 event chaired by Dr. Demby.
“Stigma and discrimination are our greatest barriers,” Lakoh stated during Monday’s events. “HIV medications are safe, effective, and life-saving—our message is clear: Get tested, seek care, and live without fear.” The government is also decentralizing pediatric ART and expanding Project ECHO training to 660 facilities across seven districts, aiming to reach underserved areas.
As Sierra Leone pushes toward ending AIDS as a public health threat by 2030, experts call for sustained international funding and local innovation.
“We’ve turned the tide on mortality, but awareness and equity must follow,” Dr. Demby urged, echoing the First Lady’s role as a UNAIDS champion for adolescent girls. With the epidemic’s heterogeneous nature—concentrated yet generalized, the nation remains vigilant, balancing celebration of milestones with the urgent work ahead.